Pregnant during the pandemic? What to expect
Pregnant During The Pandemic?
What To Expect
Joy Rojas
As COVID-19 remains a threat, CMI Obstetrics and Gynecology Specialist Joanna Lozada-Pascual explains the new ways mothers-to-be can safely navigate the next nine months.
The ongoing pandemic has not only seen a rise in COVID-19-positive cases worldwide. Strict stay-at-home orders and limited access to birth control have led to a spike in pregnancies, many of them unplanned. In the Philippines, where the “world’s longest lockdown” remains in effect, it is projected by the University of the Philippines Population Institute and the United Nations Population Fund that as many as 214,000 unplanned babies will be born this year.
Unplanned—but not unwanted—pregnancies
“A good number of pregnancies during this pandemic are unplanned—but thankfully, not unwanted,” assures Centre Medicale Internationale (CMI) Obstetrics and Gynecology Specialist Joanna Lozada-Pascual. “Couples readily take on the responsibility, but admittedly with butterflies in their stomach and with knees shaking.”
The fear and anxiety are understandable. COVID-19 remains a highly transmittable disease—and a fatal one, responsible for the deaths of over 2 million persons globally. Adding to the tension, says Dr. Pascual, is the fact that pregnant women who are of advanced maternal age, overweight, and with pre-existing health conditions like hypertension and diabetes are at high risk of experiencing severe COVID-19, and may require care in the Intensive Care Unit compared to non-pregnant women of reproductive age. “Pregnant women with COVID-19 are also more likely to experience adverse obstetric outcomes such as pre-term birth or delivery earlier than 37 weeks.”
As to whether COVID-19-positive mothers can infect their newborns with the novel coronavirus, the Centers for Disease Control and Prevention (CDC) says that while COVID-19 is uncommon in newborns born to mothers who had COVID-19, some newborns have tested positive for COVID-19 shortly after birth. It has yet to be determined if these newborns got the virus before, during, or after birth. Most newborns that tested positive for COVID-19 had mild or no symptoms and recovered.
Webinar
With still no end in sight to this pandemic (even with the presence of vaccines), doctors have taken measures to ensure that patients continue to receive optimum healthcare in these precarious times. Dr. Pascual, who recently gave the CMI webinar “Your COVID-19 Pregnancy: What Every Expectant Mother Should Know,” outlined the new normal way moms-to-be can navigate their delicate condition in the next nine months.
You’re pregnant—what now?
Upon confirming that you are indeed pregnant, the first thing you do is to call your OB-GYN, who will schedule a documentation of your pregnancy through a trans-vaginal scan. “The goal is to find out if the pregnancy is intrauterine and viable, meaning there is good fetal cardiac activity,” says Dr. Pascual.
Thereafter, expectant mothers follow a redesigned version of the prenatal system, one that keeps the mother and her unborn baby’s health and safety against COVID-19 in mind:
Telemedicine takes the place of face-to-face prenatal care visits and consultations with maternal-fetal experts and genetic counselors. Virtual consultations require a camera, microphone, a cell phone or computer, and internet connection, and come in several forms: live (a 2-way synchronous visit), store and forward (sending data or an image captured to your doctor for interpretation), hybrid visit (blends live calls with data or image transmission), and remote patient monitoring (a patient is instructed to monitor her vital signs at home and report to her doctor on the next live call).
Patient monitoring of weight, blood pressure, blood sugar, fetal heart rate, and other vital signs can be done at home and with the aid of a weighing scale, blood pressure monitor, fetal Doppler, and a glucometer.
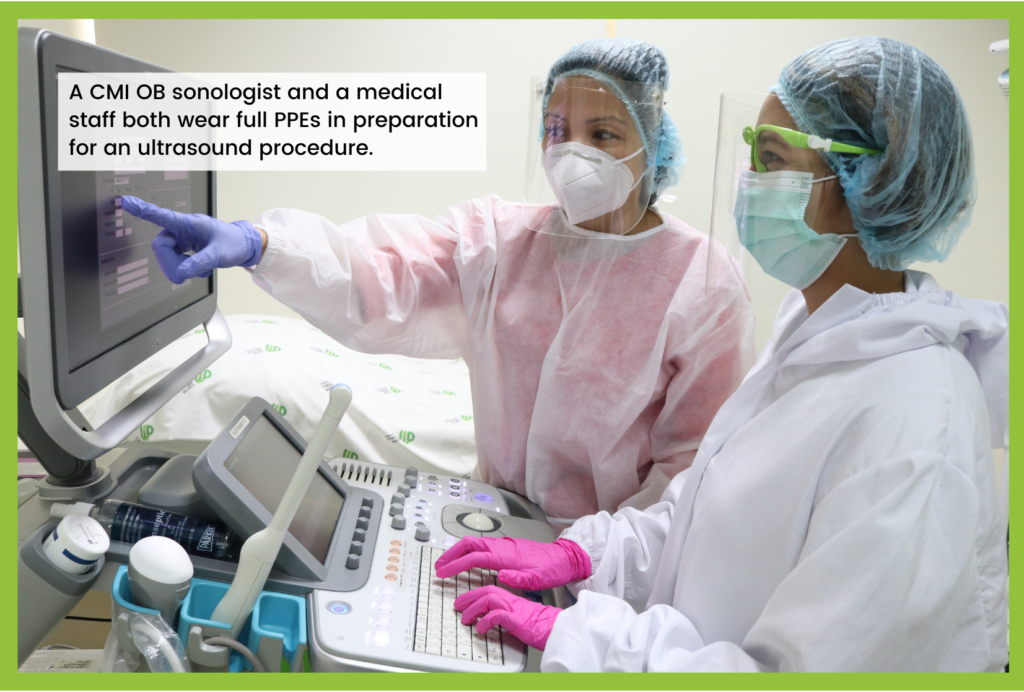
Ultrasounds require a mother to be physically present at the hospital or diagnostic center. A sonographer conducts the procedure wearing Level III personal protective equipment (PPE). The new obstetrics care model requires 1-3 ultrasounds: on the first trimester (8-14 weeks) to document the intrauterine live embryo; second trimester (20-26 weeks) to check on fetal anatomy and gender; and third trimester (35-38 weeks) to monitor fetal wellbeing, amniotic fluid, and presentation. Scanning time is limited to 15-20 minutes per patient.
“If the three scans are not feasible, the minimum recommended scan would be the fetal anomaly scan on the second trimester,” says Dr. Pascual.
Other non-negotiable tests include a complete blood chemistry, urinalysis, screenings for hepatitis B and syphilis, and fasting blood sugar, which can all be done on one visit with the proper planning.
Vaccinations benefit both mom and baby. “A pregnant woman should get vaccinated against the flu and TDAP during each pregnancy to protect herself and her baby. Immunity for baby lasts up to the first few months of life,” says Dr. Pascual. The former is given during the mother’s first in-person visit; the latter (for tetanus, diphtheria, and pertussis or whooping cough) between 27-36 weeks.
Should a pregnant woman get the COVID-19 vaccine? “Only if the risks are too high,” says Dr. Pascual. “Front-liners and healthcare workers who are pregnant are at a much higher risk of contracting the virus than the average pregnant woman, so they will definitely benefit from the vaccine.”
Facility-based deliveries require a nasopharyngeal RTP CR swab test at 37-38 weeks of a mother’s pregnancy to determine her COVID-19 status and classify her accordingly. The expectant mother is also requested to stay on strict home quarantine for 14 days after her swab test.
When deciding whether to go for a normal delivery or a Cesarean section, doctors still go by obstetric indications. “The diagnosis of COVID-19 is not at all an indication for abdominal delivery,” says Dr. Pascual.
With social distancing protocols still in place, most hospitals allow only one companion per patient. The designated companion may also have to undergo a swab test and adhere to the 14-day home quarantine, depending on the hospital where they will be having their delivery.
Rooming-in of the neonate depends on the mother’s COVID-19 status. “If the mother is COVID-19-positive but would still like to breast-feed, necessary precautions are taken,” says Dr. Pascual. “Wash your hands before breast-feeding and wear a mask.”
Early discharge of both mother and child is the goal, especially if they are COVID-19-free. A mother who underwent a normal delivery can expect to go home within 12-24 hours after delivery, while one who underwent a C-section can expect to be discharged within 24-48 hours after delivery.
Postpartum care involves monitoring mother and baby as they recuperate at home. The new mother follows instructions given in a Post-Natal Care Checklist and teleconsults with her doctor a week after delivery. “Subsequent follow-ups will depend on the needs of the patient and her baby,” says Dr. Pascual, who is also sought after as a lactation specialist. “First-time moms seek teleconsultations 1-2 times a week—and I like that because I can see that they’re really determined to become successful breast-feeders.”
Incidentally, current evidence suggests that breast-feeding is not likely to spread the virus to babies.
“Pregnancy is a special time, a pleasant life experience,” says Dr. Pascual, “but for expectant mothers facing the outbreak of the novel coronavirus, the fear and uncertainty may cloud an otherwise happy time. Please be reassured that we in the field of obstetrics, especially in the field of maternal and fetal medicine, are doing our best to deliver quality care and better patient experiences.”
With its strict adherence to safety protocols against COVID-19 and other diseases, CMI is an ideal health facility for pregnant women to undergo ultrasounds, routine laboratory procedures, and face-to-face consultations with doctors.
Over 150 physicians covering various specialties and medical needs can be accessed in the standalone urgent care clinic with its own laboratory, diagnostics and treatment room facilities. Consultations are done in luxurious and private consultation suites, and the premier health facility is on negative pressure airflow, has built-in HEPA filters, and is regularly sanitized with UVC irradiation.
To schedule an appointment at CMI, call 0927.931.7194 or email experience@cminternationale.com | Centre Médicale Internationale is at 2/F Ore Central Bldg., 31st Street corner 9th Avenue, Bonifacio Global City, Taguig City.