Advocating Home Blood Pressure Monitoring in Improving Hypertension Control
Advocating Home Blood Pressure Monitoring
In Improving Hypertension Control
By Dr. Raymond Oliva
Hypertension is an increasingly important medical and public health issue. The prevalence increases with advancing age and has come to the point that 50% of population 60 years of age, and 75% of people above 70, are affected. The Framingham Heart Study investigators reported that the lifetime risk of hypertension is approximately 90% for men and women who were nonhypertensive at age 55 or 65 years and survived to age 80-85. Data from observational studies involving 1 million individuals have indicated that death from both ischemic heart disease (IHD) and stroke increases progressively and linearly from levels as low as 115 mmHg systolic BP and 75 mmHg diastolic. For every increase of 20 mmHg systolic and 10 mmHg diastolic increase in BP, there is doubling of mortality both from IHD and stroke.
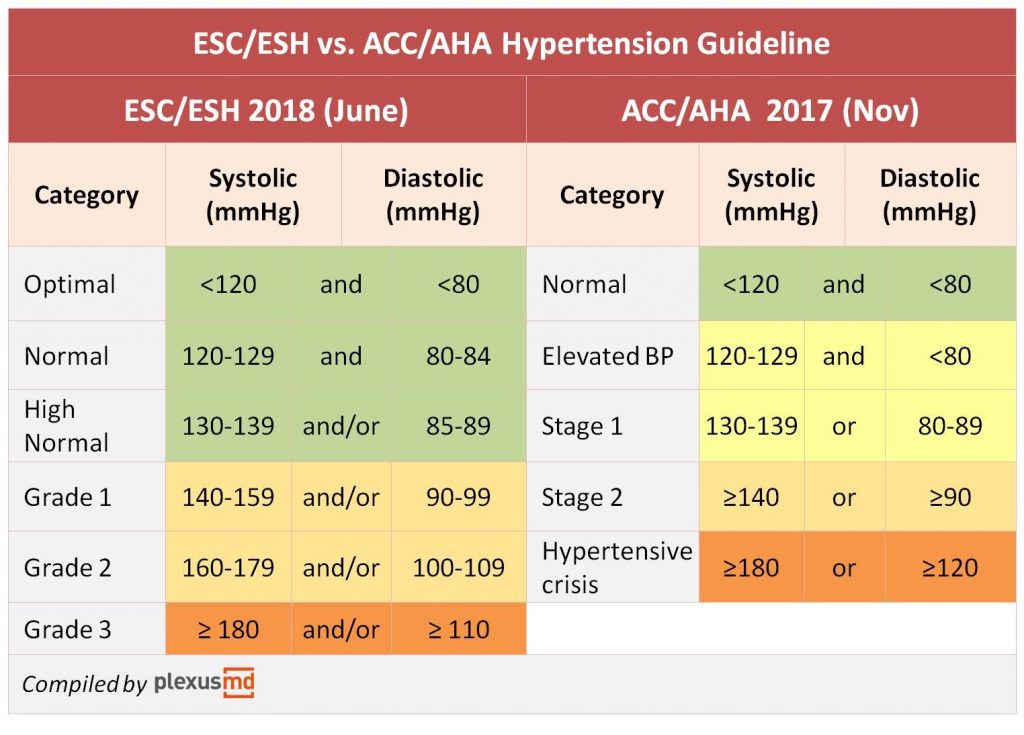
Guidelines have been formulated all over the world addressing the issue of hypertension. Two popular guidelines have come out and both have different targets (Figure 1). The American guidelines have a lower threshold of blood pressure, with stage 1 hypertension at 130/80 mmHg. The European guidelines on the other hand preferred to have BP thresholds at 140/90 mmHg.
The differences between the two guidelines stop there. Both recognize the need for better control. The control rates for hypertension remains discouraging, particularly in the Philippines. In the latest National Nutrition and Health Survey (NNHES), the prevalence of hypertension in the Philippines is 22.3% and is highest in individuals more than 70 years old. The problem with the survey is that the measurement was based only on one-time measurements done in doctors’ clinics. The use of conventional measurement of blood pressure done in the office (OBPM) has been the norm in the diagnosis and management, but this method has downsides, particularly with white coat hypertension and masked hypertension, which are quite common for both untreated and treated hypertensives. The reliability of OBPM is questioned with issues like the unstandardized setting and conditions of clinics, observer bias and errors and the small number of readings. There is also a discordance in the measurements of OBPM compared to out-of-office BP measurements which could have an effect on the “true underlying BP reading” of the individual.
Figure 1. Comparison between the ACC/AHA Guidelines vs the ESC/ESH Guidelines
Home Blood Pressure Monitoring
Home BP monitoring (HBPM) refers to the measurement of BP at home, ideally by the individual. It is optimal when the patient is seated at rest at around the same time in the morning and evening, usually a period of one week. The readings are recorded using a validated, automated BP device and is then conveyed to the physician for interpretation. This method is appealing to most patients and can lead to more awareness and control of their hypertension. HBPM allows standardization of conditions, leading to little measurement variability and reproducibility of readings. Home BP measurements can easily identify patients with white coat, masked and sustained hypertension. HBPM is also widely available and can provide day-to-day BP variability values. Despite the several advantages of HBP measurements,
it has yet to gain popularity in the Philippines because of the cost of the automated BP machines and lack of patient training.
Home Blood Pressure and its Impact on Cardiovascular Disease Management
Out-of-office BP readings taken multiple times have a better predictive value than OBPM regarding BP-related outcomes. Compared with clinic BP, HBPM has stronger associations with target organ disease. A meta-analysis examined the association of HBPM versus OBPM and ABPM, and analysis of the ten studies included showed that HBPM has a stronger correlation with echocardiographic left ventricular mass index compared to OBPM. Another meta-analysis demonstrated that HBPM is a stronger determinant of proteinuria than OBPM7.
The ultimate objective for a diagnostic method to assess a cardiovascular risk factor is its ability to predict future cardiovascular events. In prospective studies included in a meta-analysis of about 17,000 patients, HBPM showed to be superior to OBPM, and is a significant predictor of cardiovascular mortality. In the International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) study, participants with optimal or normal OBPM, hazard ratios for a composite cardiovascular endpoint associated with a 10-mmHg higher systolic HBPM were 1.28 and 1.22, respectively. At high-normal OBPM and in mild hypertension, the hazard ratios were at about 1.20 for all cardiovascular events and 1.30 for stroke. Home BP monitoring has an independent prognostic value for cardiovascular morbidity and allows for a more accurate risk stratification than OBPM.
Home Blood Pressure Monitoring for Detection of White Coat and Masked Hypertension
The use of the 24-hour ambulatory blood pressure monitoring (24 hr ABPM) is considered the gold standard in determining white-coat or masked hypertension. White coat hypertension is defined in the latest report of the American College of Cardiology/American Heart Association Task force on Clinical Practice Guidelines as higher office BP measurements than out-of-office BP readings and is considered significant if BP readings are >20/10 mmHg higher than HBPM or 24-hour ABPM. Masked hypertension, on the other hand, is defined as controlled office BP readings but uncontrolled out-of-office BP settings. The risk for cardiovascular disease and all-cause mortality with masked hypertension is similar to that with sustained hypertension and about twice as high in the abovementioned risk with normotensive patients. The inaccessibility of a 24-hr ABPM in most clinics in the Philippines makes HBPM the ideal method in detecting white coat and masked hypertension. Both methods employ multiple measurements in the usual environment of each individual, however, there are a few differences. Home BP monitoring is performed while the patient is seated and has rested for a few minutes, while the ABPM is performed in fully ambulatory conditions and postures at home, work or during sleep. However, despite these differences, average HBPM and daytime ABPM appear to have similar thresholds and diagnostic accuracy for white coat and masked hypertension.
Home Blood Pressure Monitoring and Its Impact on Blood Pressure Control
Patients who are monitoring their BP at home have been shown to improve control, with the use of HBPM associated with significant reductions in systolic and diastolic BP and reductions in antihypertensive medications compared to usual care. Advocating HBPM in hypertensive patients have reduced therapeutic inertia, which is defined as unchanged medications despite the elevation of blood pressure. However, simple home monitoring is not enough in BP control of patients. There should be interaction between the patient and their doctor. Telemonitoring has been utilized when doing HBPM, whereby the BP readings are instantly relayed to a primary healthcare professional who can guide treatment along a predetermined algorithm. The use of telemonitoring avoids travel for the patient and saves time for the healthcare team. There are some small studies suggesting that the use of HBPM may improve adherence of patients to their medications, but guidelines, such as the UK NICE guidelines still recommend a 24-hr ABPM.
Procedures for Using Home Blood Pressure Monitoring.
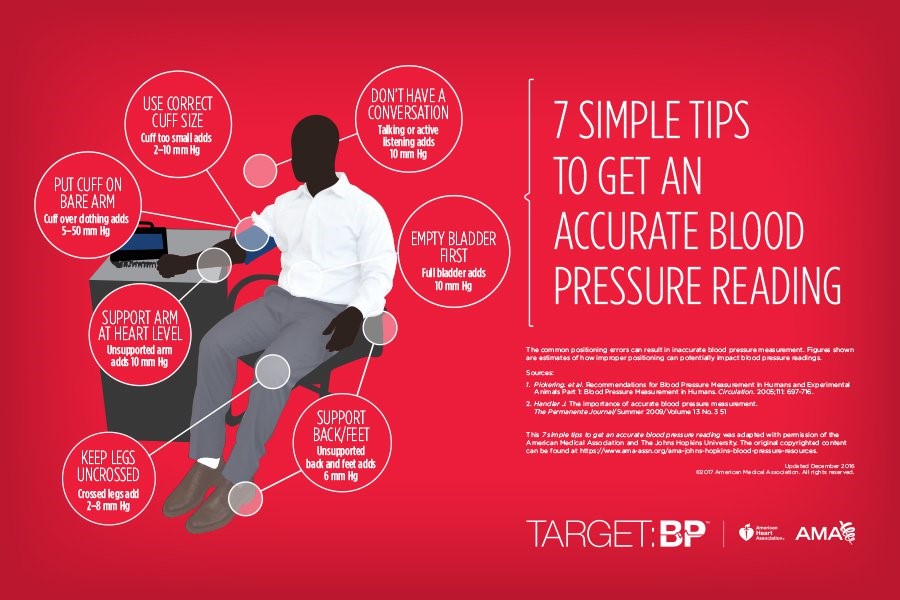
Figure 2. Tips on getting an accurate BP reading
The latest ACC/AHA guidelines for hypertension has outlined the steps in conducting BP readings at home. It is recommended that the individual should be trained by their physicians regarding information about hypertension and how to select the appropriate equipment to use. The patient should also realize that there might be variability in individual results. The physician must also educate the patient to interpret the results.
The automated device should be verified and validated. The use of auscultatory devices is not recommended as the patients may not master the technique necessary for measuring of BP. The appropriate cuff size must fit in the arm, and inter-arm differences are significant. If the differences are significant, the arm with the higher readings should be used.
During the procedure, the patient must remain still and avoid smoking, exercising or drinking coffee within 30 minutes before BP measurements. The patient must be able to rest at least 5 minutes before doing the measurements. The patient should sit correctly, with his back straight and supported, feet flat on the floor and uncrossed, and the arm supported on a flat surface. Ideally, multiple BP readings, at least 2 readings 1 minute apart before taking medications and in evening before supper should be taken. The BP should be recorded accurately and be obtained at least 2 weeks after a change in the treatment regimen and during the week before a clinic visit.
Conclusion
Office blood pressure measurements are necessary in diagnosing hypertension, but HBPM may be a necessary adjunct in establishing and monitoring BP trends and differentiating white coat and masked hypertension. We advocate the use of HBPM in Filipino hypertensive patients but should take consideration the cost of the validated machines.
Regular monitoring of your blood pressure is essential. If you are experiencing symptoms of low or high blood pressure, have yourself checked at CMI right away.
To set an appointment, contact us at 02. 8812. 1CMI | 02. 8816 .1035 – 36 or email us at experience@cminternationale.com
Literature cited
1R. Castillo, Prevalence and management of hypertension in Southeast Asia, J Hypertens, supplement 1, p. e4, 2016.
2 J. Sharman, F. Howes, G. Head, B. McGrath, M. Stowasser, M. Schlaich, P. GLasziou and M. Nelson. Home blood pressure monitoring: Australian Expert Consensus Statement. Journal of Hypertension. 2015; 33: 1721-1728.
3 J. George and T. MacDonald. Home Blood Pressure Monitoring. European Cardiology Review. 2015; 10(2): 95-101.
4Padfield PL, The case for home monitoring in hypertension, BMC Med 2010;8:55.
5Sebo P, Pechere-Bertschi A., Herrmann FR et al. Blood pressure measurements are unreliable to diagnose hypertension in primary care. Journal of Hypertension 2014; 32:509-517.
6Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens 2012; 30:449–456
7Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int. 2006; 69: 406–411.
8Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004; 329:145.
9 K. Nomura, K Asayama, L Thijs, T. Niiranen I. Luambio for the International Database of Home Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Thresholds for conventional and home blood pressure by sex and age in 5018 participants from 5 populations. Hypertension. 2014; 64: 695-701.
10 Whelton PK et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation and management of high blood pressure in adults. Hypertension 2017; 00:e000-e000.
11 R. Agarwal, J Bills, T Hecht, R. Light. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: A systematic review and meta-analysis. Hypertension 2011; 57:29-38.